A 55yr old female complains of fever,decreased appetite since 1 month, Breathlessness since 1 week,vomitings and loose stools since 3 days.
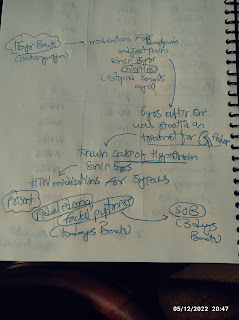
CHIEF COMPLAINTS:
Pt complains of fever,decreased appetite since 1 month, Breathlessness since 1 week,vomitings and loose stools since 3 days.
HOPI:
Patient was apparently asymptomatic 3 months back. Then she had multiple swellings in front of the left ear, for which she developed fever which was lowgrade, intermittent, no evening rise of temp, ass with decreased appetite since 1 month. She then had vomitings which was non bilious and non projectile, containing food particles. She had history of loose stools since 3 days, which is 4-5 episodes per day, watery in consistency.
Past history:
K/c/o Hypertension since 7 years.
7 yrs back she had c/o giddiness for which she went to hospital and was found to have HTN.
Personal history:
Diet- mixed
Appetite-decreased
Bowel and Bladder movements- regular.
Addictions- none
Allergies- none
General examination:
Patient is conscious, coherent and cooperative. Well oriented to time, place and person.
Moderately built and moderately nourished.
No pallor, icterus, cyanosis, clubbing, lymphadenopathy, edema.
Vitals:
Temp- 98°F
BP-110/80MMHG
RR-18CPM
PR- 74BPM.
GRBS-92mg/dl on the day of admission.
Spo2 - 100%
CNS:NAD
P/A: On Inspection:
Shape - scaphoid
Umbilicus inverted
No scars and sinuses present.
No visible pulsatios , no engorged veins
On palpation:
No rebound tenderness, no gaurding, no rigidity
No organonegaly
On percussion:
No fluid thrill
No shifting dullness
On Auscultation:
Bowel sounds heard.
Treatment:
1) IV FLUIDS(2units NS, 1unit RL) @100ml/hr.
2) INJ. NEOMOL 1GM/IV/SOS(IF temp>101°F).
3) INJ. METROGYL 100Ml/IV/TID.
4)INJ PAN 40MG/IV/BEFORE BF.
5) INJ.ZOFER 4MG/IV/OD.
6) CAP. RETODRIL 100MG/PO/TID.
7) TAB. SPORLAC-DS ,2TAB/PO/TID.
8) ORS SACHETS IN 1LITRE OF WATER, 200ML TO BE TAKEN AFTER PASSAGE OF EACH STOOL.
9)T.DOLO 650MG/PO/BD.
10) MONITOR VITALS.
11) INFORM SOS.
DIAGNOSIS:
ACUTE VIRAL GASTROENTERITIS.
K/C/O HTN SINCE 7YRS.
HIV POSITIVE (DENOVO DETECTED).














Comments
Post a Comment