A 60 year old female came to GM OPD with Chief Complaints of fever since 3 days and cough associated with sputum since 3 days.Difficulty in swallowing and pain during swallowing since 3 days, hoarseness of voice since 3 days shortness of breath since 3 days
A 60 year old female came to GM OPD with Chief Complaints of fever since 3 days and cough associated with sputum since 3 days.Difficulty in swallowing and pain during swallowing since 3 days, hoarseness of voice since 3 days shortness of breath since 3 days
HOPI:
The patient was apparently asymptomatic 3 days back then she developed high grade fever, cough with sputum which is whitish in coour non foul smelling and non blood stained. There was a history of difificult in swallowing & pain during swallowing there h/o shortness of breath 3 days back grade -II. decreased appetite since 5-6 mon ths, loss of weight since 1 year.( 20kg wt loss)
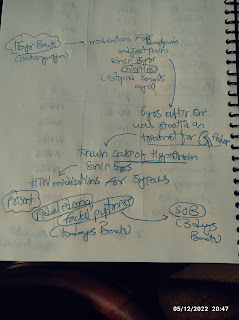
PAST HISTORY:
History of giddiness and fall ,followed by unconsciousness.
Known case of hypertension since 1 year but since 5-6 months not on regular medication . Known case of thyroid disorder since 1 year on medication. known case of DM || since ⑨ years and medication since then, tab- glibeclamide in morning, citagliptin and metformin afternoon, not a known case of epilepsy, Tb ,asthma.
No surgical history
PERSONAL HISTORY:
Diet - mixed 4 times meals per day
Appetite - decreased
Bowel and bladder - frequent micturation
Sleep - adequate,
No addictions
GENERAL EXAMINATION:
pt is ccc moderately built and moderately nourished, well oriented with place and time,
No pallor, no icterus, no cyanosis, no clubbing, no lymphadenopathy.
Vitals:
Pulse rate- 123
Bp - 110/80
Rr- 22
Temp- 99 F
Oxygen saturation 96%
Systemic examination:
CVS: no thrills ,cardiac sounds S1& S2 heard. no cardiac murmers.
Respiratory: dyspnea and wheeze present. normal vesicle breath sounds and position of the trachea central .
Abdominal examination: no soft organomegaly
CNS: NFND
Investigations
ECG
Report










Comments
Post a Comment