18 Yr female DKA with perianal absecess
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
Chief Complaints :
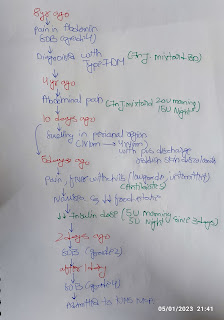
A 18 Years Old Female who is a Student Presented with C/o
- Pain & Swelling in Perianal Region Since 10days
- Fever with Chills Since 10 Days
- Shortness of Breath Since 2 Days
History of Present Illness :
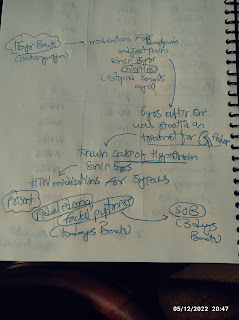
Patient Was Apparently Asymptomatic 8 Years ago then She Suddenly Developed Pain Abdomen ; Shortness of Breath (grade 4) & Lethargy for Which she went to Hospital in Hyderabad & Was Diagnosed with Type 1 DM ( RBS was around 600mg/dL ) Since then She was on Inj.MIXTARD BD.
4 Years Ago She Developed Pain Abdomen Which was Sudden Onset , Diffuse , Squeezing Type ; Non Radiating & Not Relieved With Medication & Went to Hospital Where she was told it is Due to Uncontrolled Sugars & Pain Got Subsided after Treatment & Was Prescribed with Inj.MIXTARD ( 20U - Morning ; 15U - Night )
10 Days Back She Developed Swelling Around the Perianal Region Which is Initially Around 1x1cm & Gradually Progressed to Present Size Around 4x4cm,Associated with Pus Discharge with reddish skin discoloration around the swelling , Pain, Fever with Chills 5 days back which is Low Grade & Intermittent for Which She Went to Hospital 5 Days Back & Was Started on Antibiotics. After Taking These antibiotics She Started Having Nausea & Decreased Food Intake. So They Decreased the Insulin Dose to 5U Morning & 5U Night Since 3 Days. 2 Days Back She Started Having Shortness of Breath which Was Grade 2 & GRBS Was 480mg/dl for Which She Went to Local Hospital & Took Some Injections. Then after 1 Days SOB Progressed to Grade 4 & Referred to Our Hospital.
Past History :
- H/O Swelling over inner Thighs associated with Pus Discharge 1 Year Ago Following 2nd Dose of COVID vaccination & Took Medication in local Hospital & Got Relived
- K/C/O Type 1 DM Since 8 Years
- N/K/C/O HTN ; TB ; Asthama ; Epilepsy
Personal History :
Diet : Mixed
Appetite : Decreased since 5 days
Sleep : Inadequate since 4
Bowel : not passed stools since 5 days
Bladder : regular
Addictions : Nil
Family History :
Her Father - T 2 DM Since 10 Years
GENERAL PHYSICAL EXAMINATION
Patient is conscious, coherent, coperative and well oriented to Time place and person.
She is moderately built and nourished.
No h/ o pallor, Cyanosis, clubbing, generalized lymphadenopathy - absent.
Vitals
Temperature - 98.5F
Pulse rate - 114bpm
Respiratory rate - 28cpm
Blood pressure - 120/70mm hg
SYSTEMIC EXAMINATION
•Cardiovascular system-
S1 and S2 are heard ,no murmurs are heard.
•Respiratory system:
Trachea central, all quadrants of chest moves equally with respiration. No adventitious sounds.
Breath sounds- bilateral normal
Vesicular breath sounds are heard.
•Central nervous system-
No focal neurological deficits
•Abdominal system:
Inspection:
On inspection abdomen is flat, symmetrical.
Umbilicus is centre and inverted.
All 9 regions of abdomen are equally moving with respiration.
Palpation:
On palpation abdomen is soft and mild tender.
All inspectory findings are confirmed.
Auscultation: decreased bowel sounds.
5/1/23
Provisional diagnosis: ....
Diabetics ketoacidosis with type 1 diabetes with perianal abcess
Treatment...
1) IVF - NS @100ml/HR
2) Inj HAI(0.1u/kg/hr) IV infusion
3) inj Piptaz 4.5g/IV/BD
4) inj amikacin 500mg/IV/BD
5) Inj metrogyl 100ml/iv /tid
6) GRBS monitoring hourly


























Comments
Post a Comment