1801006180 LONG CASE
This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
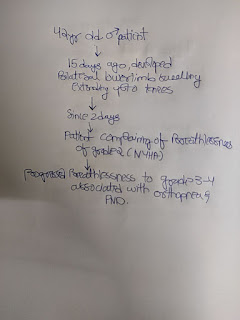
A 42 year old male patient farmer by occupation was brought to casuality with chief complaints of bilateral lower limb swelling (l>r) since 15 days, and SOB since 2 days.
HISTORY OF PRESENT ILLNESS:
•Patient was apparently asymptomatic 15 days back & then he noticed bilateral lower limb swelling which was insidious in onset gradually progressing pitting type ( left more than right ) extending up to the knees.
•Patient also complaining of breathlessness since 2 days which is Grade 2 initially progressed to Grade 3-4 (nyha)associated with orthopnea & PND
No h/o palpitations.
No h/o cough, chest pain
No h/o pain abdomen, vomiting
No h/o decreased urine output/ burning micturition ,fever and no other complaints
HISTORY OF PAST ILLNESS:
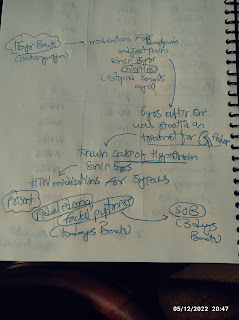
He is not k/c/o DM , HTN , Bronchial Asthma , Epilepsy CVA CAD
PERSONAL HISTORY:
Diet – Mixed
Appetite – Decreased
Sleep – Decreased (wakes up in the night once )
Bladder & Bowel movements – Regular
Addictions..He has been consuming alcohol 180ml daily , Chronic smoker 2 pack beedi/day and khaini 2-3 per day for the past 20 years.(2pack yrs)
FAMILY HISTORY
no relavant family history
TREATMENT HISTORY -
No relavant treatment history
GENERAL EXAMINATION
Patient is conscious,coherent,cooperative
Thin built & moderately nourished
Pedal edema is present
No pallor,cyanosis, clubbing, lymphadenopathy
Icterus is present.
VITALS:
1.Temperature:- 98.6 F
2.Pulse rate: 110 beats per min , regular normal volume and character
3.Respiratory rate: 18 cycles per min
4.BP: 100/70 mm Hg in right arm supine position
SYSTEMIC EXAMINATION:
A.CARDIOVASCULAR SYSTEM
Inspection:
• Chest is barrel shaped, bilaterally symmetrical.
•. JVP:Raised
• No scars or sinuses
•Apical impulse seen in left 6th intercostal space lateral to mid clavicular line.
Visible apex beat
jvpPalpation:
•All inspectory findings are confirmed:
Trachea is central, movements equal bilaterally.
•Antero-posterior diameter of chest :Transverse
diameter of chest is 1:1(approx)
•Apex beat felt in left 6th intercostal space lateral to midclavicular line
•Parasternal heave present
Auscultation:
•S1 S2 heard
•No murmurs
RESPIRATORY SYSTEM:
Inspection:
. Upper respiratory tract: no halitosis, oral thrush, tonsillitis, deviated nasal septum, turbinate hypertrophy, nasal polyp
•Chest is barrel shaped, bilaterally symmetrical.
•Trachea is central
•Movements are equal bilaterally
•Visible epigastric pulsations
•No scars or sinuses
•Apical impulse seen in left 6th Intercoastal Space lateral to mid clavicular line
Palpation:
•All inspectory findings are confirmed: Trachea is central, movements equal bilaterally.
•Apex beat felt in 6th intercostal space lateral to midclavicular line
•Vocal fremitus
Tactile vocal fremitus Right Left
Supraclavicular Resonant Resonant
Infraclavicular Resonant Resonant
Mammary Resonant Resonant
Inframammary Resonant Resonant
Axillary. Resonant Resonant
Infraaxillary decreased Resonant
Suprascapular Resonant Resonant
Interscapular Resonant Resonant
Infrascapular decreased Resonant
Percussion:
•Dull note heard in right Infra axillary area and & Infra scapular area. Right Left
Supraclavicular Resonant Resonant
Infraclavicular Resonant Resonant
Mammary Resonant Resonant
Inframammary Resonant Resonant
Axillary. Resonant Resonant
Infraaxillary dull Resonant
Suprascapular Resonant Resonant
Infrascapular dull Resonant
Interscapular Resonant Resonant
•Resonant note heard in all other areas bilaterally
Auscultation:
•Bilateral air entry present –
Normal vesicular breath sounds heard
•Breath sounds decreased in right Infra axillary area and & Infra scapular area.
•Vocal resonance decreased in right Infra axillary area and & Infra scapular area.
•Expiratory wheeze heard bilaterally.
PER ABDOMEN:
•Scaphoid
•Visible epigastric pulsations
•No engorged veins/scars/sinuses
•Soft , non tender
•No organomegaly
•Tympanic node heard all over the abdomen
•Bowel sounds present.
CENTRAL NERVOUS SYSTEM:
•HMF - Intact
•Speech – Normal
•No Signs of Meningeal irritation
•Motor and sensory system – Normal
Power tone bulk normal in all four limbs
•Reflexes – Normal
•Cranial Nerves – Intact
•Gait – Normal
•Cerebellum – Normal
•GCS Score – 15/15
.
PROVISIONAL DIAGNOSIS :
HEART FAILURE RIGHT SIDED PLEURAL EFFUSION WITH COPD
INVESTIGATIONS-
Chest x ray.
Plural fluid analysis
Volume -3ml
Appearance- clear
Colour- pale yellow
Total count- 10cells
RBC - nil
Others- nil
LIVER FUNCTION TEST
Total bilirubin 2.6mg/dl (0-1)
Direct bilirubin -1.35 mg/dl (0-0.2)
Sgot-75IU/L (0-35)
Sgpt - 31IU/L (0-45)
Alkaline phospatase -157 IU/L (53-128)
Total protiens 6.1 g/dl
Albumin 3.5
SERUM CREATININE 1.1 mg/dl ( normal 0.9-1.3)
Blood urea - 21 mg/dl
Hemoglobin - 11.3 mg/dl
ECG...
Usg findings -
right sided PLEURAL EFFUSION
2D ECHO:
Moderate to severe TR+ with PAH : mild MR+ ,
no AS/MS severe LV dysfunction.
No diastolic dysfunction,
No LV clot.
HFrEF with EF=27%(normal 50-70%)
FINAL DIAGNOSIS:
Heart failure with reduced ejection fraction (27%)? 2° to CAD Bilateral PLEURAL EFFUSION (R >L)
Copd
Treatment :
1) Fluid restriction <1lit/day
2) Salt restriction. <2gm/day
3) Tab LASIX 40mg BD (8am to 4pm)
4) Tab MET-XL 25mg BD
5) Tab ECOSPIRIN-AV 75/20 mg OD
7) BP PR temp and spO2 monitoring







Comments
Post a Comment