1801006180 SHORT CASE
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
CHIEF COMPLAINTS:
A 40 Yr old male resident of Krishnapuram, Nalgonda dist, field assistant by occupation presented with the chief complaints of:
.pain abdomen since 6 days
. nausea and vomiting since 6 days
.abdominal distention since 5 days
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 6 days ago, then he developed pain in abdomen of epigastric region which is severe, squeezing type, constant, radiating to the back and aggravated on doing any activity and relieved on sitting and bending forward.
He developed nausea and vomiting which was 10-15 episodes which was non bilious, non projectile and food as content ,and then he developed abdominal distention 5 days ago which is sudden onset, gradually progressive to current state.
no history of decreased urine output, facial puffiness,edema
no history of fever, shortness of breath, cough.
PAST HISTORY :
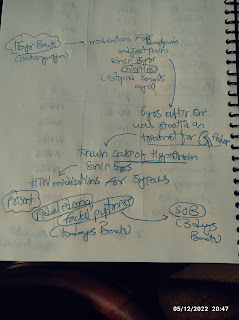
. history of diabetes since 5 years
.history of hypertension since 5 years
.no history of asthma,TB,epilepsy and thyroid disorders.
PERSONAL HISTORY:
Appetite: decreased
Diet: mixed
Sleep: adequate
Bowel and Bladder movements : regular
Addictions: history of alcohol intake for 5 years
FAMILY HISTORY:
History of diabetes to patient's mother since 14 years
History of diabetes to patient's father since 15 years
TREATMENT HISTORY:
metformin plus glimiperide
telmisartan 40 mg.
GENERAL EXAMINATION:
Patient is conscious, coherent, cooperative and well oriented to time,place and person
Moderately built and moderately nourished
Pallor - Absent
Icterus -present
Clubbing - Absent
Cyanosis - Absent
Lymphadenopathy -Absent
Pedal Edema - Absent
Vitals :
Temperature - 99 F
Pulse Rate - 80 beats per minute , Regular Rhythm, Normal In volume, No Radio-Radial or Radio-Femoral Delay
Blood Pressure - 130/90 mmHg measured in the left upper limb, in sitting position.
Respiratory Rate - 13 breaths per minute and regular
SYSTEMIC EXAMINATION:
Patient examined in a well lit room, after taking informed consent.
GASTROINTESTINAL SYSTEM EXAMINATION
Oral Cavity: Normal
Per Abdomen :
Inspection -
Shape - Uniformly Distended
Umbilicus - displaced downwards
Skin - No scars, sinuses, scratch marks, striae, no dilated veins, hernial orifices free, skin over the abdomen is smooth
External genitalia - normal.
Palpation -
No local rise in temperature, tenderness in epigastric area
Liver not palpable
Spleen not palpable
Kidneys are not palpable
Abdominal Girth - 84 cm
Xiphisternum - Umbilicus Distance - 21 cm
Umbilicus - Pubic Symphysis Distance - 15 cm
Spino-Umbilical Distance - 19 cm and equal on both sides
Percussion -
Shifting Dullness - Present
Liver dullness at 5th intercoastal space along midclavicular line - Normal
Spleen Percussion - Normal
Tidal Percussion - Absent
Auscultation -
Bowel Sounds - Absent
No Bruit or Venous Hum
CARDIOVASCULAR SYSTEM EXAMINATION
Inspection -
Chest Wall is Symmetrical
Precordial Bulge is not seen
No dilated veins, scars, sinuses
Apical impulse - Not Seen
Jugular Venous Pulse - Not Raised
Palpation -
Apical Impulse - Felt at 5th Intercostal space in the mid clavicular line
No thrills, no dilated veins
Auscultation -
Mitral Area - First and Second Heart Sounds Heard, No other sounds are heard
Tricuspid Area - First and Second Heart Sounds Heard, No other sounds are heard
Pulmonary Area - First and Second Heart Sounds Heard, No other sounds are heard
Aortic Area - First and Second Heart Sounds Heard, No other sounds are heard.
RESPIRATORY SYSTEM EXAMINATION
Inspection -
Chest is symmetrical
Trachea is midline
No retractions
No Scars, sinuses, Dilated Veins
All areas move equally and symmetrically with respiration
Palpation -
Trachea is Midline
No tenderness, local rise in temperature
Tactile Vocal Fremitus - Present in all 9 areas
Percussion - resonant all over the chest
Auscultation - normal vesicular breath sounds heard all over the chest
No added sounds
Vocal Resonance in all 9 areas- normal
CENTRAL NERVOUS SYSTEM EXAMINATION
All Higher Mental Functions are intact
No Gait Abnormalities
Signs of Meningial signs absent
Provisional diagnosis
Ascites
Investigations.
Complete blood picture
Hb 14.2 g/dl
Total count 14700
Neutrophils 90%
Lymphocytes 5%
Eosinophils 2%
monocytes 3 %
basophils 0
Platelet count 2.5 lakhs per cubic mm
Smear normocytic normochromic with neutrophilic Leukocytosis.
Liver function test
total bilirubin 2.1 mg/dl
direct bilirubin 0.6mg/dl
sgot 28iu/l
sgpt 17iu/l
alkaline phosphate 113
total protein 7.4 g/dl
albumin 4.1g/dl
A /g ratio 1.2
RBS 540 mg /dl
hbA1c 7.6%.
Ascitic fluid analysis
cell count 50 cells
Cytology negative for malignance cells
sugar 98 mg/decilitre
protein 5.1g/dl
albumin 3.3 g/dl
amylase 1055 iu/l
ADA 16IU/L
LDH 200IU/L
gram stain negative
AFB no growth
culture no growth
SAAG 0.8
serum amylase 540iu/l
serum lipase 186 iu/l
serum album 4.1 g/dl
Ascitic fluid albumin 3.3g/dl.
USG ABDOMEN :
mild to moderate ascites is seen
FINAL DIAGNOSIS:
Ascites secondary to Acute Pancreatitis
MANAGEMENT
NPO
IV Fluids - N/S
Inj. PANTOP 40 mg IV BD
Inj. ZOFER 4 mg IV SOS
Inj, PIPTAZ 2.25 mg IV TID
Tab. AMLONG 20 mg PO OD
Tab.LASIX 40 mg BD
GRBS every 4th hourly
Inj TRAMADOL 1 amp IV+100 ml NS IV OD



.PNG)
.PNG)



Comments
Post a Comment